 Introducing your baby to solid foods – sometimes called weaning or complementary feeding – should start when your baby is around six months old.It’s a really important step in their development, and it can be great fun to explore new flavours and textures together.
Introducing your baby to solid foods – sometimes called weaning or complementary feeding – should start when your baby is around six months old.It’s a really important step in their development, and it can be great fun to explore new flavours and textures together.
Three signs your baby is ready for thir first food
There are three clear signs that, together, show your baby is ready for solid foods alongside breast milk or formula. It’s very rare for these signs to appear together before your baby is six months old.
- They can stay in a sitting position and hold their head steady.
- They can co-ordinate their eyes, hands and mouth so they can look at the food, pick it up and put it in their mouth, all by themselves.
- They can swallow food. Babies who are not ready will push their food back out with their tongue, so they get more round their face than they do in their mouths.
Some signs that can be mistaken for a baby being ready for solid foods:
- chewing fists
- waking in the night when they have previously slept through
- wanting extra milk feeds
These are normal behaviours and not necessarily a sign of hunger or being ready to start solid food. Starting solid foods won’t make them any more likely to sleep through the night. Extra feeds are usually enough until they’re ready for other food.
When can I introduce weaning foods to my baby?
The World Health Organization (WHO) recommends exclusive breast feeding alone up to the age of 6 months. After 6 months babies need complementary feeding to provide adequate supply of nutrients.
Step 1: Your baby is now 6 months old (completed 6 months)
- Purées of vegetables such as carrots, pumpkin , potato, sweet potato
- Purées of fruits, such as ripe cooked apple, pear , or mashed banana
- Gluten-free baby cereals, such as rice cereal mixed with baby’s usual milk
Milk is still a major part of the baby’s diet. If you are breastfeeding, you can continue breastfeeding till baby is two years old.
Purées may be easiest for your baby at first. However, babies can quickly learn to chew soft, lumpy food even if they have no teeth. Ensure the food is well mashed and gradually make the food a thicker consistency.
Try to limit the number of sweet or cereal purées to one a day, and always include a vegetable purée.
Don’t add salt or sugar, honey or other sweeteners to your baby’s food.
Step 2: Baby is taking puréed food well
If baby is taking puréed food well, time to increase the variety in their food.
- Purées of lean meat or poultry
- Purées of lentils or split peas
- Purées of mixed vegetables with potatoes or rice
- Purées which include green vegetables, such as peas, cabbage , spinach or broccoli
- Full cream milk, yoghurt, cream cheese, paneeror custard.
Do not give cow’s (or goat or sheep’ milk) as baby’s main milk till they are atleast one year old.
Make changes in child’s diet when they are well. This is to avoid attributing the symptoms of illness to change in diet.
Some foods are more likely to cause allergies than others. These should be introduced one at a time. These foods are:
- Milk products such as cheese, yoghurt, fromage frais, paneer etc (Use full fat variety)
- Fish and shell fish
- Soya beans
- Citrus fruit (including orange juice)
- Wheat, rye and barley based foods such as bread, flour, pasta, some breakfast cereals and rusks.
- Nuts, especially if your family has a history of allergies.
Step 3: Baby food from seven to nine months
Now is the time to introduce more variety in baby’s food.
Remember that most baby food can be easily made at home.
- Mashed or minced food, not purées. Be sure to include some lumps.
- A wider range of starchy foods such as khichdi , suji upma, suji kheer, sabudaana kheer, dalia, bread. Baby breadsticks, breakfast cereals, oats, in addition to cornmeal, potatoes, rice and millet are also good options. Give two to three servings a day of starchy foods.
- Cooled, filtered and boiled waterfrom a sipper with a soft spout, when she is thirsty. This is in addition to her daily breastmilk or 500-600 mls of formula.
- Keeping juice to meal times helps with iron absorption and reduces the risk of damage to emerging teeth.
- Citrus fruits, such as oranges (santara), kinnow (keenu) and sweetlime (mosambi).
- Fish, lean red meat, poultry and lentils. Aim for one serving of protein-rich food a day.
- Nut butters as long as there is no family history of allergic diseases. Use unsalted smooth versions, or make your own.
- Dairy products, such as paneer, yoghurt and cheese. You should wait until one year to introduce cow’s milk as a drink. However, it can be used in small amounts for cooking foods.
- Follow-on formula, if you wish.
- Finger foods such as cooked green beans (frans been) or carrots (gajar), cubes of cheese, slices of banana (kela) or soft pear (nashpati).
If you are buying canned food, do ensure they do not contain excess salt or sugar. Adult canned food is not recommended for babies as it contains excess salt or sugar.
Step 4: Meals from 10 months
Meals should be more adult-like now. They should be chopped or minced. You may like to follow a two to three meal a day pattern along with one or two snacks. Continue to offer breastmilk or 500-600mls of formula milk.
At this stage your baby should be having:
- three or four servings of starchy foods, such as khichdi, rice, dal, dalia, or potatoes, a day
- one serving of meat, fish, well-cooked eggs, or two of pulses (lentils, peas, beans) or nut butters
- one to two servings of cheese, paneeror yoghurt as well as breastmilk or formula milk.
What foods should I not give my baby if she is under a year?
- Salt: Adding salt to baby food is neither needed nor recommended in the first year of life
- Honey. Even if she has a cough, your baby shouldn’t have honey until she’s one.
- Sugar. Try sweetening desserts with mashed banana or a purée of stewed dried fruit. Or you could use expressed breast milk or formula milk.
- Artificial sweeteners. Diet drinks or squashes containing artificial sweeteners are not suitable for your baby. They are not nutritious and can encourage a<style=”color: #000000;”>sweet tooth.
- Whole nuts.These are a choking hazard.
- Tea or coffee. The tannin in tea may prevent her from absorbing the iron in her food properly. Any caffeinated drink is unsuitable for your baby.
- Low-fat foods. Single or double toned milk, yoghurts and reduced-fat cheeses aren’t right for your baby. Always offer your baby the full-fat versions. She needs the calories.
- Foods which may carry a risk of food poisoning; such as soft mould-ripened cheeses (brie, camembert), liver pâté, and soft-boiled or raw eggs.
- Cow’s (or goat’s or sheep’s) milkas a main drink under one year.

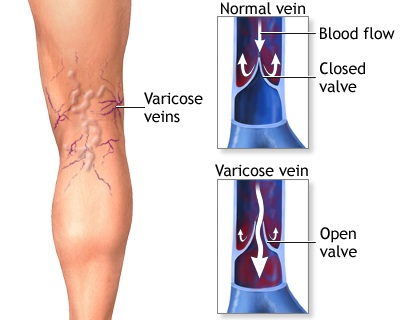
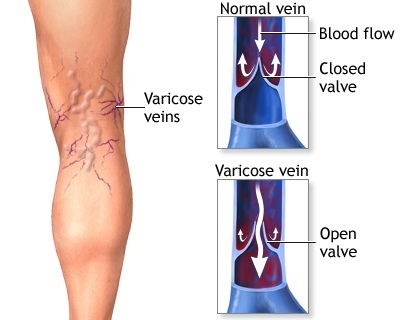 Varicose veins are swollen, twisted, and enlarged veins that you can see under the skin. They are often red or blue in color. They usually appear in the legs, but can occur in other parts of the body.
Varicose veins are swollen, twisted, and enlarged veins that you can see under the skin. They are often red or blue in color. They usually appear in the legs, but can occur in other parts of the body.