Gestational diabetes is a condition in which your blood sugar level becomes high during pregnancy, affecting up to 10% of pregnant women, diagnosed by a blood test done at 24 to 28 weeks of pregnancy. Women with gestational diabetes don’t have diabetes before their pregnancy – and it usually goes away after giving birth.
What causes gestational diabetes?
Hormones produced by the placenta cause a build-up of glucose in the blood. Usually, enough insulin is produced to control blood sugar levels. However, if the body is unable to produce insulin or stops using it, then the blood sugar levels rise, causing gestational diabetes.
Who’s at risk of gestational diabetes?
At your first antenatal appointment, a healthcare professional should check if you’re at risk of gestational diabetes.
The likelihood of getting gestational diabetes increases if you:
• were overweight before you got pregnant.
• have had gestational diabetes in the previous pregnancy.
• have had a large baby in earlier pregnancy (4.5kg/10lb or more)
• have a family history of diabetes – parent or sibling.
• come from a South Asian, Black or African Caribbean or Middle Eastern background.
• have high blood pressure .
• have given birth to a stillborn baby.
• are older than 30 years.
Having gestational diabetes increases your risk of developing it again in future pregnancies. It also increases your risk of developing Type 2 diabetes later in life. You can reduce the risk of developing gestational diabetes by managing your weight, eating healthily and keeping active before pregnancy.
Gestational diabetes symptoms.
Women with gestational diabetes don’t usually have symptoms. Most find out that have it during a routine screening.
You may notice that:
• You’re thirstier than usual
• You’re hungrier and eat more than usual
• You urinate more than usual
Gestational diabetes tests and diagnosis.
Gestational diabetes is diagnosed by routine screening, called Oral Glucose Tolerance Test, also known as an OGTT. The OGTT is done when you’re between 24-28 weeks pregnant. If you’ve had gestational diabetes before, you’ll be offered an OGTT as soon as possible, and another OGTT between 28-32 weeks if the first test result is normal.
How do you manage gestational diabetes?
The goal is to reduce blood glucose to the normal levels exhibited by a woman without gestational diabetes.
This involves:
• Measuring your blood sugar level four times a day
• Eating a healthy and balanced diet
• Performing moderate physical activity for about 150 minutes per week (Running, walking and swimming are good options)
• Reducing stress as much as possible.
These measures must be taken while continuing regular checkup with your doctor and adjusting them as needed. Changes in habits will sometimes not be enough; in such cases, metformin or insulin injections should be used during the pregnancy.
Target blood sugar levels in pregnancy:
• Before a meal: 95mg/dl or less
• An hour after a meal: 140mg/dl or less
• Two hours after a meal: 120mg/dl or less
Tips for eating well with gestational diabetes:
• Eat regular meals.
• There’s no need to ‘eat for two’. Portion size will have the most significant effect on your blood glucose level.
• Include carbohydrates but look for low GI (glycemic index) options and keep the consumption to the optimum level
• Get your five vegetables a day for vitamins, minerals and fibre.
• Cut back on salt, too much salt is associated with high blood pressure, which increases the risk of diabetes complications.
• Stick to water or sugar-free drinks.
What are the potential complications?
In the child:
• Macrosomia (above-average weight)
• Risk of being born with low blood sugar levels and respiratory problems
• Risk of obesity and type 2 diabetes later in life
In the mother:
• Risk of a difficult delivery, possibly by C-section, depending on the baby’s weight
• Surplus of amniotic fluid, which could trigger premature delivery
• Gestational hypertension & Preeclampsia
• Risk of developing type 2 diabetes later
• Risk of suffering from gestational diabetes again in a future pregnancy
Most of the complications can be prevented with appropriate treatment.
In conclusion, in the vast majority of cases, gestational diabetes is easy to control, with your blood sugar levels likely to normal in about six weeks after childbirth. However, the risk of developing gestational diabetes in the next pregnancy increases, with the women also likely to develop type 2 diabetes in the future. It would help if you got follow-up tests every year. Many problems can be avoided through healthy lifestyle habits. Don’t panic and talk to your doctor to see how you can put the odds in your favour.

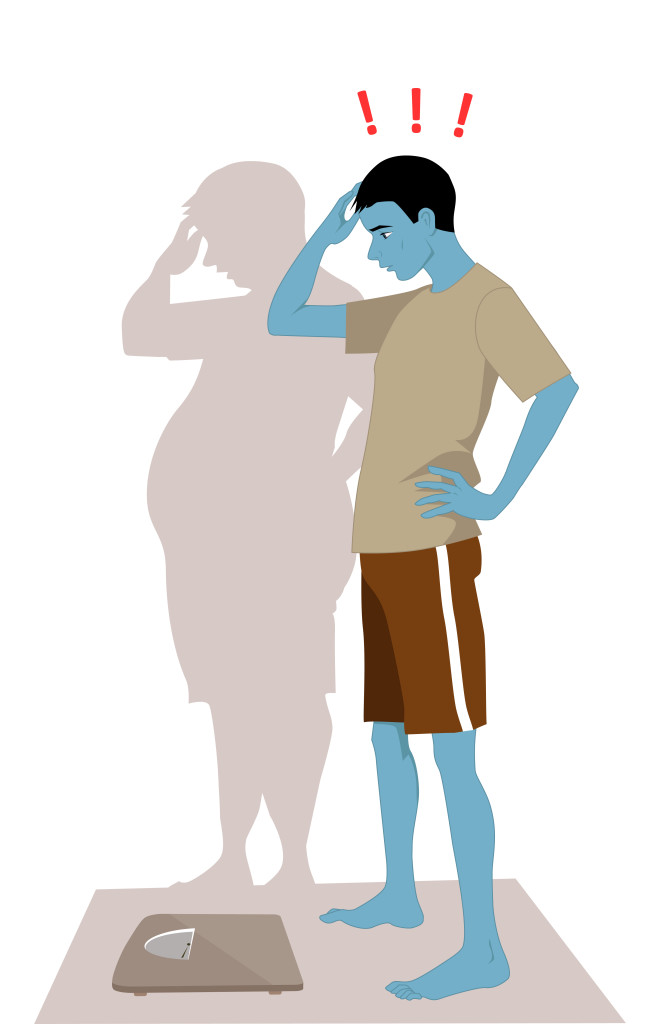 Anorexia Nervosa is a psychological and possibly life-threatening eating disorder defined by an extremely low body weight relative to stature (this is called BMI [Body Mass Index] and is a function of an individual’s height and weight), extreme and needless weight loss, illogical fear of weight gain, and distorted perception of self-image and body.
Anorexia Nervosa is a psychological and possibly life-threatening eating disorder defined by an extremely low body weight relative to stature (this is called BMI [Body Mass Index] and is a function of an individual’s height and weight), extreme and needless weight loss, illogical fear of weight gain, and distorted perception of self-image and body.
 hemoglobin and cardiac and nerve and brain damages.
hemoglobin and cardiac and nerve and brain damages.