What is hysteroscopy?
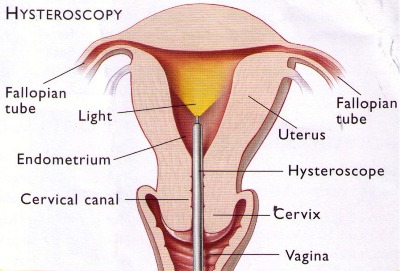
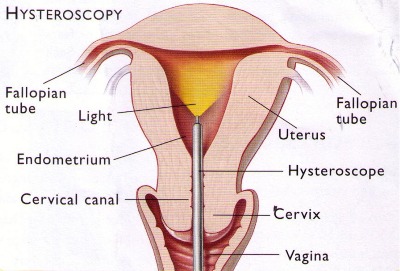
Hysteroscopy is a procedure that allows a doctor to look inside the uterus in order to diagnose and treat causes of abnormal bleeding. Hysteroscopy is done using a hysteroscope – a thin, lighted tube that is inserted into the vagina to examine the cervix and inside of the uterus.
Why is hysteroscopy done?
One of the most common uses for hysteroscopy is to find the cause of abnormal uterine bleeding. Abnormal bleeding can mean that a woman’s menstrual periods are heavier or longer than usual or occur less often or more often than normal. Bleeding between menstrual periods also is abnormal. Hysteroscopy may be either diagnostic or operative.
What is diagnostic hysteroscopy?
Diagnostic hysteroscopy is used to diagnose problems of the uterus such as abnormal uterine bleeding, infertility, repeated miscarriages, adhesions, fibroids, polyps, or to locate displaced intrauterine devices (IUDs). It may also be used to confirm the results of other tests such as hysterosalpingography (HSG). Other instruments or techniques, such as dilation and curettage (D&C) and laparoscopy, are sometimes used in conjunction with the hysteroscopy.
What is operative hysteroscopy?
Operative hysteroscopy is used to correct an abnormal condition that has been detected during a diagnostic hysteroscopy, avoiding the need for a second surgery. During operative hysteroscopy, small instruments used to correct the condition are inserted through the hysteroscope.
When is operative hysteroscopy used?
Hysteroscopy may be performed to correct the following uterine conditions:
- Polyps and fibroids – Hysteroscopy is used to remove these non-cancerous growths found in the uterus.
- Adhesions – also known as Asherman’s Syndrome, uterine adhesions are bands of scar tissue that can form in the uterus and may lead to changes in menstrual flow as well as infertility. Hysteroscopy can help locate and remove the adhesions.
- Septums – Hysteroscopy can help determine whether you have a uterine septum, a malformation of the uterus that is present from birth.
- Infertility – tubal blockage at uterine end can be opened through hysteroscopy by cornual cannulation
- Abnormal bleeding – Hysteroscopy can help identify the cause of heavy or lengthy menstrual flow, as well as bleeding between periods.
- Postmenopausal bleeding – Hysteroscopy is also performed to determine the cause of unexplained bleeding or spotting in postmenopausal women
- Removal of foreign body or a missing IUCD
What are the benefits of hysteroscopy?
Compared with other, more invasive procedures, hysteroscopy may provide the following advantages:
- Shorter hospital stay
- Shorter recovery time
- Less pain medication needed after surgery
- Avoidance of hysterectomy
- Possible avoidance of “open” abdominal surgery
How safe is hysteroscopy?
Hysteroscopy is a relatively safe procedure. However, as with any type of surgery, complications are possible. With hysteroscopy, complications occur in less than 1 percent of cases and can include:
- Risks associated with anesthesia
- Infection
- Heavy bleeding
- Injury to the cervix, uterus, adjacent organs
- Intrauterine scarring
When should the procedure be performed?
It may be recommended to schedule the hysteroscopy for the first week after your menstrual period. This timing will provide the doctor with the best view of the inside of the uterus.
What type of anesthesia is used for hysteroscopy?
Anesthesia for hysteroscopy may be local, regional, or general:
How is hysteroscopy performed?
Prior to the procedure, one may be prescribed a medication to help you relax. You will then be prepared for anesthesia. The hysteroscope is inserted through vagina and cervix into the uterus. Saline is then inserted into the uterus, through the hysteroscope, to expand it and to clear away any blood or mucus. A light shone through the hysteroscope allows the doctor to see inside the uterus and the openings of the fallopian tubes into the uterine cavity. Finally, if surgery needs to be performed, small instruments are inserted into the uterus through the hysteroscope.
The time it takes to perform hysteroscopy can range from less than 5 minutes to more than an hour. The length of the procedure depends on whether it is diagnostic or operative and whether an additional procedure, such as laparoscopy, is planned at the same time.
How will I be prepared for hysteroscopy?
If you are having general anesthesia in the hospital, you will be told not to eat or drink anything for a certain period of time (usually after midnight the night before) before the procedure. Routine lab tests may be ordered as well for women having a hysteroscopy in the hospital. You will be asked to empty your bladder and your vaginal area will be cleansed with an antiseptic
What can I expect after the procedure?
If regional or general anesthesia is used during your procedure, you may have to be observed for several hours before going home. After the procedure, you may have some cramping or slight vaginal bleeding for one to two days. However, if you experience any of the following symptoms, be sure to contact your doctor:
- Fever
- Severe abdominal pain
- Heavy vaginal bleeding or discharge
Will I have to stay in the hospital overnight?
Hysteroscopy is considered minor surgery and usually does not require an overnight stay in the hospital. However, in certain circumstances, such as if your doctor is concerned about your reaction to anesthesia an overnight stay may be required.
Who is a candidate for this procedure?
Although there are many benefits associated with hysteroscopy, it may not be appropriate for some patients. A doctor who specializes in this procedure will consult with your primary care physician to determine whether it is appropriate for you.








 It is important for these people to see a Surgeon at the earliest to enable an accurate diagnosis and initiate early treatment to prevent further complications. Over the counter medications and creams are of limited use as almost all of these conditions present with more or less the same complaints, however the treatment is completely different for each one of them.
It is important for these people to see a Surgeon at the earliest to enable an accurate diagnosis and initiate early treatment to prevent further complications. Over the counter medications and creams are of limited use as almost all of these conditions present with more or less the same complaints, however the treatment is completely different for each one of them. These however, need to be performed by experienced Surgeons who have undergone extensive training in this specialty and have the know how and technical expertise.
These however, need to be performed by experienced Surgeons who have undergone extensive training in this specialty and have the know how and technical expertise. Approximately 20% of the UAE population suffers from Chronic Sinusitis. Symptoms range from stuffy nose, nasal blockage, headache, facial pain, postnasal discharge, cough and bad breath. These are all symptoms of chronic sinusitis. The weather in UAE plays a significant role in the development of these symptoms. Fine sand in the air, humidity, allergies, sudden temperature changes too trigger it. Deviation of the nasal septum and nasal polyps too can lead to chronic sinusitis.
Approximately 20% of the UAE population suffers from Chronic Sinusitis. Symptoms range from stuffy nose, nasal blockage, headache, facial pain, postnasal discharge, cough and bad breath. These are all symptoms of chronic sinusitis. The weather in UAE plays a significant role in the development of these symptoms. Fine sand in the air, humidity, allergies, sudden temperature changes too trigger it. Deviation of the nasal septum and nasal polyps too can lead to chronic sinusitis. Visual inspection, nasal endoscopy and CT scan, paranasal sinuses can help screen for chronic sinusitis. A CT scan can accurately diagnose chronic sinusitis. Once diagnosed, it is treated with nasal decongestants, steroid nasal sprays, antihistamines, antibiotics etc.
Visual inspection, nasal endoscopy and CT scan, paranasal sinuses can help screen for chronic sinusitis. A CT scan can accurately diagnose chronic sinusitis. Once diagnosed, it is treated with nasal decongestants, steroid nasal sprays, antihistamines, antibiotics etc. Pain may be classified into different types based on the origin, duration, periodicity and nature of pain. Accordingly, Pain management can broadly be classified as acute and chronic pain management. While acute pain deals with perioperative pain, pain in labour, trauma, burns etc., and the latter includes a diverse group of patients in the outpatient setting. The management of acute pain is primarily therapeutic. Chronic pain management requires various pharmacological and non pharmacological approaches to tackle the multidimensional components of pain. At International Modern Hospital we take a holistic approach so as to not only treat the underlying cause but also provide psychological support and rehabilitation to ailing patient.
Pain may be classified into different types based on the origin, duration, periodicity and nature of pain. Accordingly, Pain management can broadly be classified as acute and chronic pain management. While acute pain deals with perioperative pain, pain in labour, trauma, burns etc., and the latter includes a diverse group of patients in the outpatient setting. The management of acute pain is primarily therapeutic. Chronic pain management requires various pharmacological and non pharmacological approaches to tackle the multidimensional components of pain. At International Modern Hospital we take a holistic approach so as to not only treat the underlying cause but also provide psychological support and rehabilitation to ailing patient. Pain management largely comprises of pharmacological and non-pharmacological modalities, commonly being medication, counselling, relaxation techniques, electrical stimulation and local anaesthetics. Few Prescribed medications include anti-depressants and systemic local anaesthetics.
Pain management largely comprises of pharmacological and non-pharmacological modalities, commonly being medication, counselling, relaxation techniques, electrical stimulation and local anaesthetics. Few Prescribed medications include anti-depressants and systemic local anaesthetics. At International Modern Hospital we undertake Interventional modalities which include diagnostic and therapeutic nerve blocks, facet blocks, epidural steroids, intra articular injections, trigger point injections for myofacial syndromesetc. Therapeutic adjuvants include Psychiatric counselling, physiotherapy and electrical stimulation. Unrelieved and inadequate relief of pain is continuing to be a global health problem and serious efforts have to be taken to provide pain treatment as it is definitely a basic human right.
At International Modern Hospital we undertake Interventional modalities which include diagnostic and therapeutic nerve blocks, facet blocks, epidural steroids, intra articular injections, trigger point injections for myofacial syndromesetc. Therapeutic adjuvants include Psychiatric counselling, physiotherapy and electrical stimulation. Unrelieved and inadequate relief of pain is continuing to be a global health problem and serious efforts have to be taken to provide pain treatment as it is definitely a basic human right.