The incidence of Cancer both benign and malignant is on the rise worldwide. Cancer treatment especially for malignancy can damage or disfigure the body parts function and or appearance. Reconstructive Plastic Surgery helps to repair the damage and restore near normal appearance.

Unlike Cosmetic Surgery, most insurance companies cover Reconstructive Plastic surgery.
Reconstructive surgery is usually needed after a tumour is removed and there is a defect which needs to be covered. E.g. after Mastectomy ( surgical removal of breast) for cancer- the patient may choose to have the breast volume restored . Or after a jaw tumour when the onco-surgeon has removed one side of the jaw bone and cheek completely and there is a huge open defect.

Reconstructive Surgery can be performed immediately after removal of the tumour (Immediate reconstruction) or can be performed after completion of other cancer treatments like chemotherapy and radiation therapy (Delayed Reconstruction).
Reconstructive surgery can make use of several body parts solely or in combination to facilitate good reconstruction. Options of reconstruction may include use of only skin (skin graft) or flap surgery ( combination of skin, fat , muscle or bone).
With the advancement in Microsurgery and techniques, single stage reconstruction with good cosmesis is possible. It works by taking tissue and blood vessels from one part of the patient’s body and placing it over the damaged part and joining the vessels under the operating microscope.
All options of reconstruction are to be discussed with the reconstructive plastic surgeon before surgery.
Reconstructive Surgery is no longer a social taboo, but a way forward to a better quality of life and better future.


 It is important for these people to see a Surgeon at the earliest to enable an accurate diagnosis and initiate early treatment to prevent further complications. Over the counter medications and creams are of limited use as almost all of these conditions present with more or less the same complaints, however the treatment is completely different for each one of them.
It is important for these people to see a Surgeon at the earliest to enable an accurate diagnosis and initiate early treatment to prevent further complications. Over the counter medications and creams are of limited use as almost all of these conditions present with more or less the same complaints, however the treatment is completely different for each one of them. These however, need to be performed by experienced Surgeons who have undergone extensive training in this specialty and have the know how and technical expertise.
These however, need to be performed by experienced Surgeons who have undergone extensive training in this specialty and have the know how and technical expertise. Approximately 20% of the UAE population suffers from Chronic Sinusitis. Symptoms range from stuffy nose, nasal blockage, headache, facial pain, postnasal discharge, cough and bad breath. These are all symptoms of chronic sinusitis. The weather in UAE plays a significant role in the development of these symptoms. Fine sand in the air, humidity, allergies, sudden temperature changes too trigger it. Deviation of the nasal septum and nasal polyps too can lead to chronic sinusitis.
Approximately 20% of the UAE population suffers from Chronic Sinusitis. Symptoms range from stuffy nose, nasal blockage, headache, facial pain, postnasal discharge, cough and bad breath. These are all symptoms of chronic sinusitis. The weather in UAE plays a significant role in the development of these symptoms. Fine sand in the air, humidity, allergies, sudden temperature changes too trigger it. Deviation of the nasal septum and nasal polyps too can lead to chronic sinusitis. Visual inspection, nasal endoscopy and CT scan, paranasal sinuses can help screen for chronic sinusitis. A CT scan can accurately diagnose chronic sinusitis. Once diagnosed, it is treated with nasal decongestants, steroid nasal sprays, antihistamines, antibiotics etc.
Visual inspection, nasal endoscopy and CT scan, paranasal sinuses can help screen for chronic sinusitis. A CT scan can accurately diagnose chronic sinusitis. Once diagnosed, it is treated with nasal decongestants, steroid nasal sprays, antihistamines, antibiotics etc. Pain may be classified into different types based on the origin, duration, periodicity and nature of pain. Accordingly, Pain management can broadly be classified as acute and chronic pain management. While acute pain deals with perioperative pain, pain in labour, trauma, burns etc., and the latter includes a diverse group of patients in the outpatient setting. The management of acute pain is primarily therapeutic. Chronic pain management requires various pharmacological and non pharmacological approaches to tackle the multidimensional components of pain. At International Modern Hospital we take a holistic approach so as to not only treat the underlying cause but also provide psychological support and rehabilitation to ailing patient.
Pain may be classified into different types based on the origin, duration, periodicity and nature of pain. Accordingly, Pain management can broadly be classified as acute and chronic pain management. While acute pain deals with perioperative pain, pain in labour, trauma, burns etc., and the latter includes a diverse group of patients in the outpatient setting. The management of acute pain is primarily therapeutic. Chronic pain management requires various pharmacological and non pharmacological approaches to tackle the multidimensional components of pain. At International Modern Hospital we take a holistic approach so as to not only treat the underlying cause but also provide psychological support and rehabilitation to ailing patient. Pain management largely comprises of pharmacological and non-pharmacological modalities, commonly being medication, counselling, relaxation techniques, electrical stimulation and local anaesthetics. Few Prescribed medications include anti-depressants and systemic local anaesthetics.
Pain management largely comprises of pharmacological and non-pharmacological modalities, commonly being medication, counselling, relaxation techniques, electrical stimulation and local anaesthetics. Few Prescribed medications include anti-depressants and systemic local anaesthetics. At International Modern Hospital we undertake Interventional modalities which include diagnostic and therapeutic nerve blocks, facet blocks, epidural steroids, intra articular injections, trigger point injections for myofacial syndromesetc. Therapeutic adjuvants include Psychiatric counselling, physiotherapy and electrical stimulation. Unrelieved and inadequate relief of pain is continuing to be a global health problem and serious efforts have to be taken to provide pain treatment as it is definitely a basic human right.
At International Modern Hospital we undertake Interventional modalities which include diagnostic and therapeutic nerve blocks, facet blocks, epidural steroids, intra articular injections, trigger point injections for myofacial syndromesetc. Therapeutic adjuvants include Psychiatric counselling, physiotherapy and electrical stimulation. Unrelieved and inadequate relief of pain is continuing to be a global health problem and serious efforts have to be taken to provide pain treatment as it is definitely a basic human right.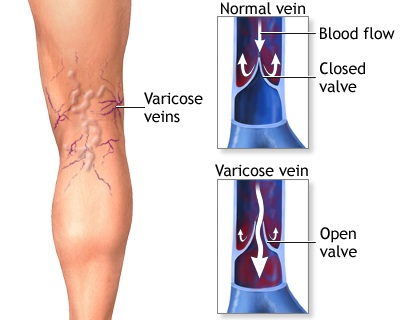
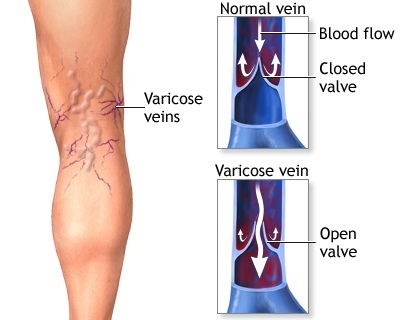 Varicose veins are swollen, twisted, and enlarged veins that you can see under the skin. They are often red or blue in color. They usually appear in the legs, but can occur in other parts of the body.
Varicose veins are swollen, twisted, and enlarged veins that you can see under the skin. They are often red or blue in color. They usually appear in the legs, but can occur in other parts of the body.

